
"I say yes to research because it is important to contribute to the community and share your views, and to advocate for people who are less able to raise their voices and be heard."
– Virginia Chiu, Richmond
It is a moment that Virginia Chiu will never forget. A passenger in a car-totalling accident, Chiu was rushed to the nearby Richmond Hospital emergency department.
“I remember waiting on the hospital bed, hooked up to so many machines and not feeling well,” recalls Chiu, who has lived in Richmond, B.C., her entire life. The injury, which occurred in the mid-2000s, ended up being non-life-threatening, although Chiu was left with a lingering knee injury.

That experience and others informed Chiu’s decision to participate in the Novel Emergency Waiting-room Sensing for Safety (NEWS²) study, which investigated two novel vital signs monitoring devices for patients waiting in the emergency department. Led by Vancouver Coastal Health Research Institute (VCHRI) researcher Dr. Kendall Ho, along with Drs. Hashim Kareemi and Barinder Brar, the technology has the potential to support optimal patient care while easing some of the burden on health care staff.

Twenty years following Chiu’s accident, emergency departments in British Columbia are facing increased pressure from an expanding population with more complex medical needs, along with a health care staffing crunch. The situation has resulted in longer emergency room wait times — up from around three hours across B.C. in 2019 to four hours and 13 minutes in 2024 — and is something that Chiu and her family have experienced.
“My husband and I took our daughter to the emergency department when she developed a high fever and was projectile vomiting,” Chiu shares. “She was still very young, around three years old, and could not communicate, so we did not know what was wrong.”
“We waited for over seven hours in the emergency department before she could be seen by a physician. We also waited about that long when my husband dislocated his finger.”
These experiences informed Chiu’s decision to sign up for the NEWS² study. “I learn a lot from participating in health care research,” says Chiu, who has volunteered for other VCHRI studies in the past.
A support system for emergency department triage staff
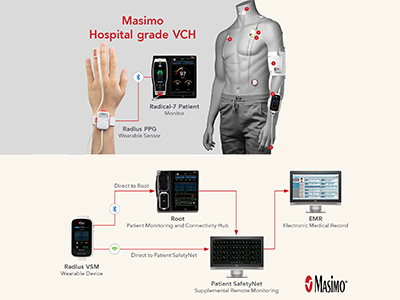
NEWS² study participants had to have previously visited an emergency department to receive care or accompanied someone receiving care. When participating in the study in 2025, Chiu was asked to wear two novel medical-grade vital signs monitoring equipment prototypes configured by the research team.
One prototype that was wrapped around Chiu’s finger monitored her oxygen saturation as well as heart rate, while the second prototype — worn on Chiu’s chest and hand — monitored her oxygen saturation, heart rate, blood pressure and body temperature.

The devices connected via Bluetooth to a monitor that was hardwired to the central, secure digital system used by triage nurses in the emergency department. This connectivity meant that participants needed to stay within range of the monitor while donning the devices.
Chiu was guided through the Richmond Hospital emergency department with research team members to simulate real-world scenarios.
“I acted out the process of washing my hands, as I would following using the washroom,” Chiu relays. “The devices could not get wet at the time, so I had to take them off. The one worn around the finger was harder to remove and put back on.”
“The chest and hand device had more wires, but was easier to remove and replace,” adds Chiu. “It was also more comfortable. Plus, I would not mind having more hanging things like wires to have more vital signs monitored.”

Following around 30 minutes in the emergency department, Chiu filled out a questionnaire provided to her by the research team, sharing essential feedback on the user experience. These insights will inform the next phase of this research involving trialling the technology on a selection of patients awaiting care in emergency departments.
“The goal is to provide triage staff — the first points of contact and ongoing monitors of patients entering the emergency department and awaiting care — with real-time data to identify patients whose conditions are worsening, allowing for faster and more timely care,” notes Ho.

A portable, wearable vital signs monitoring device could also relieve some of the pressure on emergency care staff, offering another safe and effective checkpoint to monitor patients awaiting further testing, consultation or care.
“This technology is something that would be most beneficial for patients who are not displaying symptoms when they arrive at the emergency department, but who are at high-risk of developing symptoms,” says Ho. “For example, it could be worn by an individual with a history of heart disease who arrives in hospital with shortness of breath but no chest pain.”
Armed with insights from research participants and care staff, researchers are planning to launch a feasibility trial of upgraded portable, wearable NEWS² vital signs monitoring technology in 2026.
This is one patient's story of participating in a research study. Your experience may differ. Learn about clinical trials before participating.


