Curiosity leads to world’s first trial of deep brain stimulation for spasmodic dysphonia.
Vancouver Coastal Health Research Institute scientist and neurosurgeon Dr. Christopher Honey had treated hundreds of Parkinson’s patients’ tremors using deep brain stimulation (DBS) when he and his team became curious about whether DBS could be used to treat a different condition also characterised by involuntary muscle movements—spasmodic dysphonia (SD). Affecting the muscles of the larynx, SD causes individuals to have a choppy, hoarse or strained-sounding voice. Looking at past patient files, the researchers followed up with two individuals who underwent DBS to treat a tremor, but also had SD at the time.

“We were delighted and surprised to hear that the patients experienced significant improvement with their voice after DBS,” says Honey. “We weren’t aware that had happened but the patients said, ‘I thought that was part of the deal!’ That was the first indication ever that DBS might also help SD.”

In adductor SD, which makes up the vast majority of SD cases, the brain sends incorrect signals to the muscles controlling the vocal cords causing them to close involuntarily, restricting airflow and making it difficult to talk.
DBS involves the implantation of electrodes in targeted areas of the brain. Thin wires connect the electrodes to a pacemaker-like device, typically placed under the skin in the chest area, that generates electrical pulses to the electrodes to modify the abnormal signals from the brain that are causing involuntary muscle spasms. The pulse-generating device can be turned on and off by an external remote control.
Currently, the most common treatment for SD is botulinum toxin injections (i.e. Botox®). While the injections reduce the intensity of vocal cord spasms and allow for more normal speaking, side effects can include near-paralysis of the voice initially after treatment, difficulty swallowing and weakness of the throat. Botox® treatments need to be repeated every three to four months and the injection itself is uncomfortable, requiring the needle to go through the neck and precisely into the affected muscles of the larynx.
“Botox® is unfortunately just a temporary downstream fix that addresses the throat muscles even though there’s nothing wrong with them,” he says.
“SD is the brain misfiring and our study is directed at addressing the underlying, neurological cause of the disorder.”
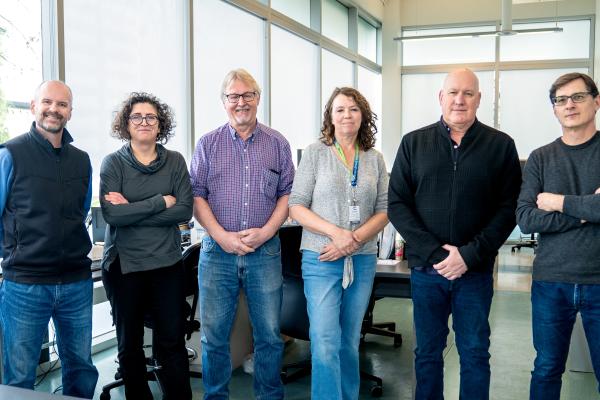
Honey is leading the world’s first clinical trial looking at using DBS for the SD. The study—Deep Brain Stimulation for Spasmodic Dysphonia—also known as the DEBUSSY trial, included six patients with SD and who did not have a tremor. The patients were randomized to have their DBS turned on or off without them knowing during the three-month blinded phase of the study. Participants were then crossed over to the other setting for another three months. Their subjective quality of life and an objective measure of their voice was recorded after each three-month period.
While data from the study is still being analyzed, Honey shares that results thus far are promising. No patient had any adverse effects from the surgery.
Restoring voices and quality of life
Honey notes that the DBS effect was so powerful that even though patients were not aware what was happening step-by-step during their treatment, they knew when the DBS device was on because they were talking normally and they knew when it was off because their voice was spasmodic.
“That DBS may effectively treat SD means possibly improving patients’ everyday lives.”
“SD can really affect a person’s quality of life in terms of their voice being so poor that they can’t work or their friends and family can’t understand them,” explains Honey. “While we don’t think that everyone with SD needs DBS, patients who cannot manage comfortably with medication or Botox® may now have an effective treatment option.”