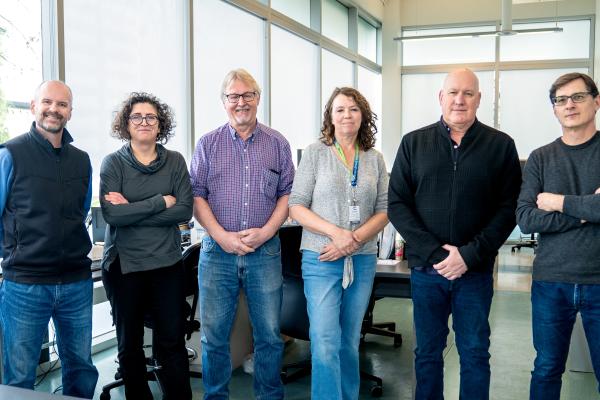
Congratulations to the recipients of the 2025 Innovation and Translational Research Awards.
Taking innovative research from concept to application is critical for improving health care systems and well-being of patients. Vancouver Coastal Health Research Institute (VCHRI) is proud to support investigators and their groundbreaking health research with the Innovation and Translational Research Awards. This year’s recipients are putting new knowledge into practice, implementing research outcomes and turning discoveries into commercial opportunities.
The 2025 Innovation and Translational Research Award recipients are:
- Dr. Thalia Field, stroke neurologist and associate professor in the Department of Medicine at UBC
- Dr. David Granville, professor in the Department of Pathology and Laboratory Medicine at UBC
- Dr. Gillian Hanley, associate professor in the Department of Obstetrics and Gynaecology at UBC
- Dr. Joanne Matsubara, professor in the Department of Ophthalmology and Visual Sciences at UBC
- Dr. Jessica Moe, emergency physician and assistant professor in the Department of Emergency Medicine at UBC
- Dr. Stephanie Sellers, assistant professor in the Department of Medicine at UBC
- Dr. Marie-Pier St-Laurent, urologist and assistant professor in the Department of Urologic Sciences at UBC
- Dr. Cheryl Wellington, professor in the Department of Pathology and Laboratory Medicine at UBC
 Can a novel application for perfusion brain scans help improve outcomes for rarer stroke types?
Can a novel application for perfusion brain scans help improve outcomes for rarer stroke types?

Study: Perfusion imaging to guide personalized acute therapy in cerebral venous thrombosis
Cerebral venous thrombosis (CVT) is a type of stroke that most commonly affects young women and can lead to lasting, life-altering symptoms. Even with medical treatment, over one-third of people who experience CVT will be unable to return to work due to cognitive issues, pain, seizures and other complications.
Dr. Thalia Field is studying how computed tomography perfusion — a routine type of brain scan used to evaluate patterns of blood flow during a stroke — may be applied to identify CVT patients at greatest risk of developing the most serious complications following a CVT stroke. Field hopes that this research will help to better guide treatment decisions when CVT patients first present to hospital.
“This work will help to improve outcomes after CVT, and may impact care delivery both locally and internationally,” says Field. “Our research could support the optimization of limited hospital resources in addition to greater positive outcomes for patients and their loved ones.”
 A novel curative and preventative treatment for bed sores
A novel curative and preventative treatment for bed sores

Study: A novel multi-pronged approach to treating pressure injuries
Immobility and prolonged pressure on the skin and underlying tissues can lead to pressure injuries, also called bed sores. Once healed, the skin affected by these wounds rarely returns to its original strength, resulting in increased risk of recurring, non-healing wounds in the same place. Pressure injuries are a major cause of comorbidity and mortality in aging, obese and immobilized populations. As such, pressure injuries pose a significant health challenge and economic burden for long-term care facilities and hospitals.
Dr. David Granville has identified a multi-pronged approach to treat these wounds. His lab previously discovered a tissue-degrading enzyme, Granzyme B, that is elevated in pressure injuries and impedes normal wound healing. When this enzyme is inhibited, wound healing and tissue remodeling markedly improve. The research team has evidence that inhibition of Granzyme B could inhibit both onset and progression, as well as recurrence of pressure injuries, and has recently identified natural compounds that inhibit Granzyme B that would be ideal for treating these debilitating wounds. In a second independent study, Dr. Granville's team has also identified a safe, clinically approved drug that, in addition to reducing infection, reduces pressure injury onset and severity by promoting blood flow in wounded tissue.
“Our new approach will involve investigations into understanding how these compounds work in order to advance the development of novel treatments for pressure injuries,” says Granville. “We are highly optimistic that this combined therapeutic strategy could provide affordable, safe and effective options for treating pressure injuries.”
Improving pregnancy outcomes for people with endometriosis

Study: Improving our understanding of associations between endometriosis treatments and pregnancy outcomes
Endometriosis is an incurable condition in which uterine tissues grow outside of the uterus. Endometriosis can cause life-altering pain, difficulties becoming pregnant as well as an elevated risk of complications during pregnancy.
Despite the fact that endometriosis affects one in 10 people of reproductive age with a uterus, little is known about the relationship between endometriosis treatments and pregnancy. Dr. Gillian Hanley’s research will examine the relationship between different endometriosis treatments and successful conceptions as well as complications during pregnancy.
“In the process of collecting data on endometriosis treatments and patient outcomes among individuals attempting to conceive and individuals experiencing pregnancy, we will work closely with our endometriosis patient partners to develop the best ways to communicate our results,” says Hanley. “This collaborative approach can help to ensure that endometriosis patients planning for a future pregnancy are better equipped to make informed decisions about different treatment options with their health care providers.”
Treating eye diseases with non-invasive eye drops

Study: Innovative drug delivery by eye drop system for retinal diseases
Age-related macular degeneration (AMD) is a serious eye disease and common cause of vision loss in older adults. The condition is associated with a protein called vascular endothelial growth factor (VEGF), which induces the growth of abnormal blood vessels in the eye, leading to cell damage and potentially blindness if left untreated.
The current intervention for AMD involves injecting a special medication directly into the eye to block VEGF. While injections are effective, they come with risks such as bleeding, retinal detachment or infection. They also require frequent clinic visits, placing added burden on patients and the health care system. Dr. Joanne Matsubara’s study aims to develop a non-invasive, anti-VEGF eye drop that would offer an alternative treatment to injections. The eye drops would temporarily and safely lower cell barriers in the eye, allowing the anti-VEGF medication in the eye drops to permeate cell barriers and enter deep into the eye without causing long-term damage.
“There is a clear need for a better way to deliver these medications that would be safer, more convenient and less stressful for patients,” says Matsubara. “Developing an eye drop would be a significant advancement to alleviate the clinical burden and improve patients’ quality of life.”
Supporting people who use drugs in emergency departments

Study: Promoting safety and equity in chaos: A feasibility study of peer support workers to support people who use drugs in emergency departments
Many people with high-risk opioid use visit emergency departments (EDs). These patients are at greater risk of dying compared to other patients, especially if they leave before being discharged from hospital after completing the recommended course of medical care. Integrating peer support workers into EDs could improve safety and comfort for people who use substances based on peers' shared experience. However, ED peer programs for people with opioid use have not been widely studied in Canada.
Dr. Jessica Moe will work closely with operations leads at Vancouver General Hospital who are leading the implementation of the first peer support worker program at VGH for people who use non-medical opioids. Her team will provide assistance with design and planning of the program, including thoughtful screening procedures and peer support worker scheduling. Peer workers will make regular rounds of the ED and waiting room and will receive referrals from providers. They will help build rapport and facilitate communication between patients and health care providers. The focus of Moe’s study will be feasibility evaluation and estimation of the program’s effectiveness at decreasing patients who leave before medically advised, to set the foundation for a future study across Canada.
“This study will assess the feasibility of ED peer support workers with lived experience to improve care, equity and outcomes for patients who use non-medical opioids,” says Moe. “Our learnings will assist other EDs that are designing and rolling out similar peer programs with the potential to improve the care of patients with high-risk opioid use on a national scale.”
Expanding treatment options for patients with heart valve disease

Study: Optimizing outcomes for patients with heart valve disease through leaflet modification
Replacement of diseased heart valves with an artificial valve is the main recommended treatment for heart valve disease. Coronary artery obstruction is a life-threatening complication of valve replacement that occurs when the artificial heart valve implant pushes aside the diseased valve flaps, called leaflets, which then block blood flow to the heart muscle. Fortunately, there are various methods to modify diseased leaflets and prevent coronary artery obstruction, called leaflet modification (LM). However, there is currently limited research comparing LM techniques and few opportunities for clinicians to learn how to use these techniques.
Using ex-vivo modelling, Dr. Stephanie Sellers’s project will compare different LM techniques, including electrosurgical and mechanical, to evaluate their safety and effectiveness. The research team will also develop an educational laboratory setup to expand training options for clinicians and increase availability of these techniques. This will include an interactive digital workbook, a repository of recorded live cases of LM techniques and a bench-top model that gives clinicians an opportunity to practice LM.
“The project will provide the means to improve skills of care providers wanting to use LM techniques in their practice,” says Sellers. “This work provides important scientific insight and learning opportunities regarding LM techniques, making us more knowledgeable about these new LM techniques and ultimately allowing us to advance treatment options for patient with heart valve disease.”
Reducing the need for invasive bladder surgeries with improved patient selection

Study: Investigating the use of bladder MRI and utDNA to detected clinical complete responder following neoadjuvant therapy for muscle-invasive bladder cancer
Bladder cancer that invades the muscle layer around the bladder requires aggressive treatment, including chemotherapy followed by potentially life-saving surgery to remove the bladder. However, in 30 to 40 per cent of cases, pathology reports of removed bladder tissues reveal that the cancer had already been eradicated by the chemotherapy.
Dr. Marie-Pier St-Laurent’s clinicial trial, NEO-BLAST, focuses on improving the identification of patients whose bladder cancer was eliminated during chemotherapy and who may not need to receive bladder removal surgery. In collaboration with Drs. Gillian Vandekerkhove and Ren Yuan, St-Laurent will investigate the use of two innovative diagnostic tools to evaluate the presence of bladder cancer post-chemotherapy treatment: a novel form of a urine test that looks to identify tumour DNA in a patient’s urine sample (utDNA), and radiomics analysis that combines special image analyses incorporating artificial intelligence and MRI picture of the bladder.
“This research could transform bladder cancer care by offering to patients personalized treatment options that reduce the need for surgery if they have a complete response with the chemotherapy, potentially avoiding invasive procedures and hospital stays,” says St-Laurent. “Additionally, the unique utDNA test that has been developed at the Vancouver Prostate Center has the potential to become a simple and convenient urine test that could make this innovation accessible to patients worldwide.”
Exploring a blood test to accurately diagnose traumatic brain injury in children

Study: Using the Alamar NULISA technology to discover diagnostic and prognostic biomarkers in pediatric traumatic brain injury
Computed tomography (CT) imaging is the primary method used for diagnosing traumatic brain injury (TBI) in children. While effective, this diagnostic tool involves radiation and sedation, which can be stressful for young children, thus highlighting the need for alternative low-cost, non-imaging options to improve diagnosis of mild TBI and prognosis of severe TBI in children.
Dr. Cheryl Wellington’s research seeks to determine whether a blood test could help doctors diagnose and treat kids with TBI. Leveraging Alamar’s NULISA technology — a state-of-the-art proteomic liquid biopsy platform for ultra-high sensitivity and broad biomarker profiling — Wellington will analyse a large dataset and existing blood samples from pediatric patients who experienced TBI to identify patterns that could be used to create the alternative diagnostic tool. The research team will use the Alamar panel to profile 120 biomarkers and determine which biomarkers can improve diagnostic precision for pediatric TBI across the severity spectrum. As the Alamar test only requires a tiny volume of blood, this research could pave the way for a finger prick test to be used in the future for children who have sustained a TBI.
“TBI is the leading cause of acquired disability in children, and early, accurate diagnosis is key to mitigate TBI-associated negative social and cognitive impairments,” says Wellington. “This study will use first-in-Canada technology that can take a tiny drop of blood to help improve the diagnosis and prognosis of pediatric TBI.”
Innovation and Translational Research Awards are made possible with the generous support of the VGH & UBC Hospital Foundation and Providence Research in partnership with VCHRI.