
A rapid tissue assessment technology dramatically reduced surgical times, making possible real-time biopsy analysis and enhanced accuracy.
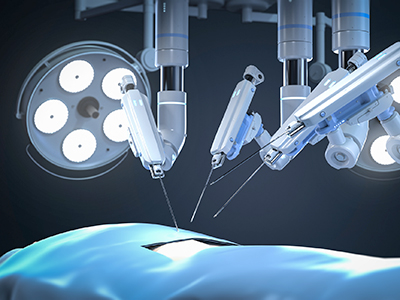
A technology used in advanced brain and lung cancer surgery is now being explored in the removal of prostate cancer. The first-of-its-kind study — led by Vancouver Coastal Health Research Institute researcher Dr. Miles Mannas — applied cutting-edge stimulated Raman histology (SRH) to rapidly analyze tissue biopsies during robotic radical prostatectomy, significantly reducing surgical times while enhancing cancerous tissue removal.
“SRH brings pathology into surgeons’ hands,” says Mannas. “We anticipate that this technology could significantly reduce the risk of cancer recurrence in the surgical area.”

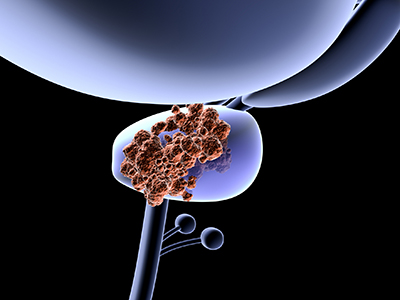
SRH is akin to a computerized, portable pathology team. It rapidly produces high-quality and high-resolution images of tissue biopsies, such as those taken from a surgical site. To identify the presence of disease indicators in tissue biopsies, SRH’s built-in computer algorithm leverages advanced artificial intelligence (AI) to sift through and compare biopsies to pre-loaded data sets of, for example, prostate cancer cells. The technology is currently used clinically at centres in the United States and in Europe, but is not yet approved for use in Canada.
Streamlined processes to reduce surgical time and enhance patient outcomes
In their recent paper, Mannas and his team reviewed the performance of SRH paired with advanced robotic-assisted laparoscopic radical prostatectomy (RALP).
Mannas and his team first developed and trained an SRH AI algorithm to identify prostate cancer in tissue biopsies for a previous study — drawing from images of about 300 biopsies from 100 prostate cancer patients. In his more recent study, Mannas and his team retrained the algorithm on biopsies from 12 RALP patients, testing its accuracy on the biopsies of an additional 10 RALP patients.
When paired with SRH, RALP technology enables surgeons to quickly extract biopsies from the surgical site for rapid, real-time analysis under the SRH unit’s powerful optical microscope within the operating room.
“A major advantage of SRH technology is that it makes tissue assessment possible without the need to involve pathology teams, reducing the burden on the health care system and operating rooms.”
The standard of care for margin assessment without SRH involves sending biopsies from surgical margins to in-hospital pathology labs for analysis. “The current, non-SRH pathology workflow is resource-, time- and labour-intensive,” Mannas says. “Tissues need to be processed by histology experts, which includes sectioning and staining, and reviewed by a pathologist.”
This process typically takes about 70 minutes to complete, contributing to the total surgical time of the procedure.
SRH, on the other hand, returned results with 100 per cent margin assessment accuracy within around four minutes, adding virtually no extra time to the surgical process. In other words, the SRH AI that Mannas and his team developed was able to perfectly discriminate cancer infiltrated margins from cancer-free margins in a fraction of the time normally required for this process.
“The possibility to drastically reduce the length of RALP, and potentially other surgeries, could help address the current patient wait times of up to one year for this procedure.”
Another major advantage of SRH is its application in real-time decision making in the operating room. For major surgeries like RALP, surgeons must decide on how much tissue to remove from the surgical site based on the results of routine biopsies taken during the surgical procedure and their knowledge of long-term treatment outcomes.
“Stimulated Raman histology gives us more opportunities to make informed treatment decisions.”
With the rapid tissue assessment capabilities of SRH, surgeons can review more biopsies during surgery, providing more touchpoints to assess whether enough cancer has been removed from surrounding tissues and preserving as much vital, healthy tissue as possible.
“Surgeons are always balancing the risks and rewards of how much tissue to remove at the margins of a tumour,” shares Mannas. “SRH gives us more opportunities to make informed treatment decisions.”
The next phase of Mannas’s research will be to ground truth SRH in clinical settings through additional clinical trials, he says. “This technology is the future because it is faster and also very accurate.”


