New research underscores the role of estrogen and genetics, calling for more sex-stratified studies and tailored treatment approaches.
Heart disease risk may have more to do with genetic factors interacting with sex hormones than previously thought, according to the findings of a new study led by Dr. Tara Sedlak, a Vancouver Coastal Health Research Institute researcher and one of the only certified women’s heart health cardiologists in Canada. Published in Frontiers in Cardiovascular Medicine, the study found evidence of under-explored genetic risk of cardiovascular disease connected to estrogen, a steroid hormone that plays an important protective role in female cardiovascular health.
“As estrogen levels change, so too does the risk of cardiovascular disease.”
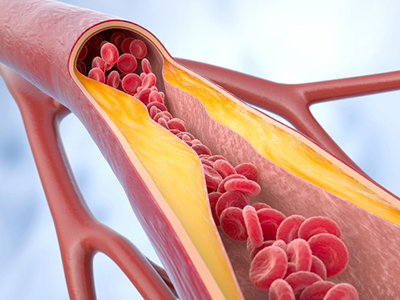
Estrogen reduces inflammation in the body and helps to maintain blood vessel dilation, among other protective effects. Estrogen levels are highest and most protective during the reproductive years, gradually declining with the onset of perimenopause and menopause, which typically occur in a person's 40s and 50s, respectively.

These changes in hormone levels can affect everything from cholesterol to body fat distribution.
“As females age, their metabolism changes,” explains Emilie Théberge, a UBC medical genetics PhD student and co-first author of the study with UBC medical student Ava Aminbakhsh. “Their bodies are more prone to holding onto fat. Muscle mass is more important to retain bone strength. They are also more prone to higher cholesterol and osteoporosis, and the list goes on.”

Estrogen levels can change from monthly fluctuations during pregnancy; conditions affecting hormones, such as polycystic ovarian syndrome; or with medications, such as birth control, fertility treatments or menopausal hormone therapy.
Getting adequate exercise and sleep, and maintaining a healthy diet and weight, can all stave off some of the ill effects of lower estrogen. However, further research is needed to understand exactly how hormone level changes impact heart disease risk among individuals who, for example, have a history of female-specific conditions or use certain medications, says Théberge. Answering these questions could better inform which medical interventions should be introduced and when.
Understanding the connection between genes and hormones to unlock precision treatments
Sedlak and Théberge’s review focused on genetic differences known as single nucleotide polymorphisms (SNPs), which are small changes in the genetic code. You can be born with SNPs or they can arise over time due to aging and other environmental factors.
“Estrogen affects over 2,000 genes in the body — everything from how certain proteins are expressed to the functioning of cells.”
“If your complete genome — the 23 pairs of chromosomes you inherit from your parents — is a recipe book, and each gene is a recipe, SNPs are changes akin to spelling errors in one of the recipes,” shares Théberge. “Polygenic risk is like if a recipe calls for sugar when it should say salt. Many of these changes are small and have little impact in isolation; however, as a whole, an accumulation of these changes can increase the risk of heart disease.”
“For comparison, monogenic disease genes are the larger effects of SNPs that can be thought of as ripping out a page from a recipe,” Théberge adds. “SNPs in these genes are also rarer and can have more severe health consequences. When we talk about individuals with a genetic heritable predisposition to heart disease, we are often referring to monogenic risk factors.”
Family history of disease should be discussed with one’s doctor as it is an important proxy for assessing genetic risk in the absence of genetic testing, Théberge advises.
A call to action for hormone data to be included in heart studies
Sedlak and Théberge’s research identified 36 coronary artery studies that had genome-wide significant SNPs linked to 61 genes. Of these, only three studies reported on significant SNPs from sex-specific analyses mapped to genes.
Importantly, within the 36 relevant studies, 26 genes were found to be modulated by estrogen and discussed in depth. Some of those genes were identified as playing a role in heart disease markers, such as lipid synthesis, metabolism, lipoprotein mechanisms, vascular integrity and thrombosis — blood clots in the blood vessels or heart.
“This demonstrates a direct link between how estrogen levels can impact heart disease risk at the genetic level, and is an area that has been historically understudied in scientific research and not always factored in for treatment development in clinical trials,” Théberge explains.
“Our findings are a call to action for researchers in the field of cardiovascular disease to include hormone data in their studies, such as through sex stratification and female-specific variables in study design.”
With a growing body of sex-specific evidence, Théberge believes that new tailored heart treatment avenues, including personalized precision medicine approaches and lifestyle changes, could be pursued for women whose estrogen levels are in a state of flux.
“Drug companies, researchers and doctors need to be aware of how estrogen levels may change the side effects and efficacy of the medications presently indicated for female heart patients, including gold-standard medications that affect blood pressure or cholesterol levels,” says Théberge. “We need more research in this space to offer science-backed recommendations for the effective treatment of female patients with heart disease at all stages of life.”