An implantable, rapid alert system streamlines tissue flap monitoring, enabling quick action to save surgical flaps and avert additional surgeries.
A new implantable tissue monitoring technology could be a gamechanger for complex head and neck reconstructive surgery, as well as other surgeries. Developed by Vancouver Coastal Health Research Institute (VCHRI) researchers Drs. Babak Shadgan and Donald Anderson, the microvascular free tissue transfer Near-Infrared Spectroscopy (FTT-NIRS) sensor system could reduce the number of revision surgeries needed for invasive skin flap transplants.
“Our technology is a custom, miniaturised version of an advanced Near-Infrared Spectroscopy (NIRS),” Shadgan explains. “It can monitor real-time tissue hemodynamics — circulation within tissues in the form of tissue pulsations — and the level of tissue oxygenation, alerting care teams should these systems become compromised.”

“Vascular surgeries could greatly benefit from a sensor like this,” adds Anderson, who has performed microvascular free graft surgery for 41 years.
“This technology could be a gamechanger for a variety of surgical procedures.”
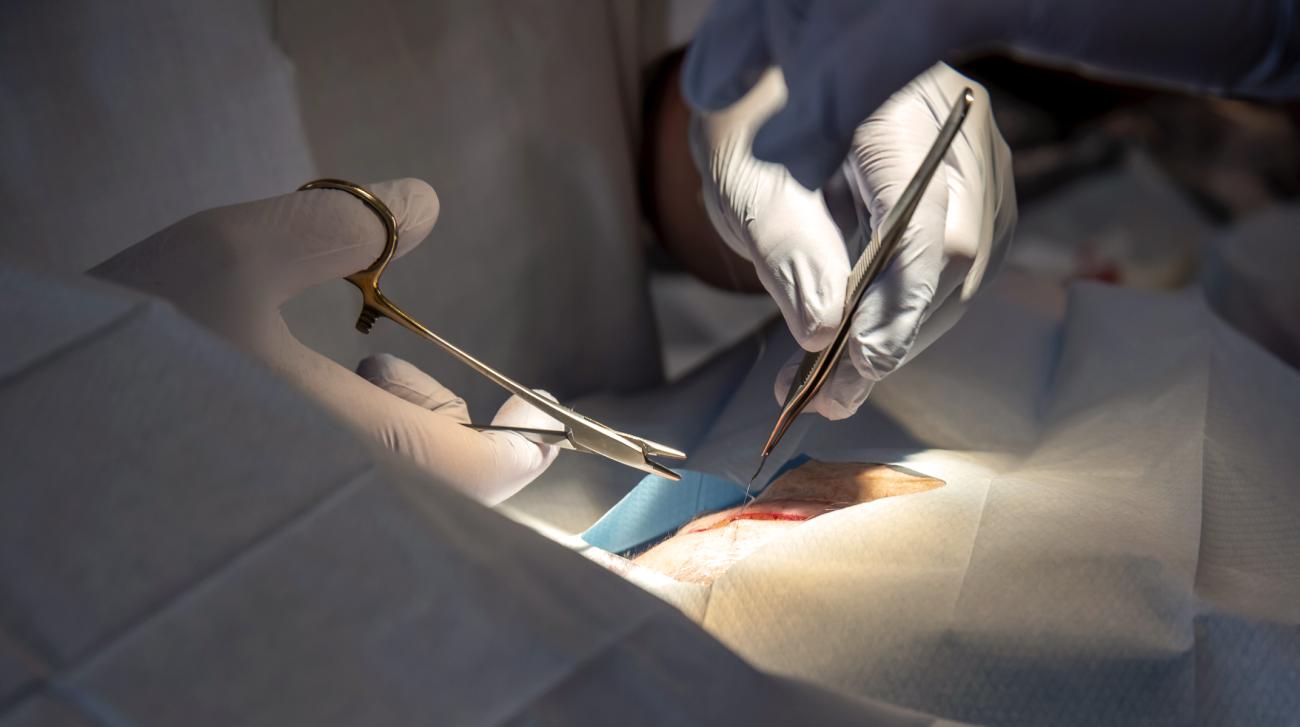
Shadgan and Anderson’s research is looking specifically at the application of the FTT-NIRS sensor and emitter probes in free flap head and neck surgery involving skin tissue sourced from another part of the patient’s body. Complex surgical procedures like this can be required for patients with head or neck cancer or other conditions that require the removal of skin, muscle and potentially bone from the head or neck.
Donor flap tissue taken from the patient must contain arterial and venous connection points to hook up to the arteries and veins at the implant site. Compromised or lost transplanted tissue blood flow often stems from a blocked artery or vein in the graft, such as from a blood clot. Flap emergencies from vascular compromises like this are rare, occurring around four per cent of the time, but have a significant impact on patients and health care providers.

“The critical determinant of flap survival often lies in the immediate postoperative period,” Shadgan explains. “During this vulnerable window, vascular compromise, if not promptly detected, can lead to irreversible flap loss within a few hours, necessitating reoperation and exposing patients to serious complications.”
Attached by wires to a nearby computer, the FTT-NIRS system monitors tissue vital signs for up to 72 hours post-surgery, covering a period in which the risk of graft failure is highest.

Once placed over or implanted within the surgical site, the waterproof FTT-NIRS probes emit near-infrared light — up to two centimetres into tissues — using small, optical sensors that monitor flap hemodynamics and oxygenation. The degree of near-infrared light absorbed by oxygenated and deoxygenated hemoglobin — an iron-rich protein found in red blood cells — supplies the FTT-NIRS algorithm with the necessary data to determine whether tissue oxygenation is too low or tissue circulation is compromised.
Objective, accurate and real-time monitoring of high-risk tissues
Without FTT-NIRS, visual tissue monitoring is conducted at regular intervals by hospital staff. If tissue compromise is suspected, specialised clinicians are called on to determine whether urgent surgical intervention is needed.
“We can get a call in the middle of the night because the tissue flap has lost blood flow,” Anderson shares. “When that happens, immediate action is necessary to save the flap. If the tissues die, a revision surgery is essential, but many factors can impede it, including operating room or donor tissue availability.”

“Free flap head and neck surgeries can take anywhere from four to eight hours,” adds Anderson. “This is to say nothing about the impact having to undergo another surgical procedure on the head or neck can have on patients and treatment outcomes.”
The FTT-NIRS sensor provides continuous, objective data, reducing hospital staff time spent checking tissues using subjective and less precise measures, such as tissue colour and capillary refill time. Whenever tissue compromise is detected, the FTT-NIRS sensor sends an alert to care providers for rapid assessment and intervention.
Anderson explains and demonstrates some of the key benefits of the FTT-NIRS in this video:
Credit: Dr. Babak Shadgan (scientist), Dr. Oleksandr Butskiy (surgeon) and Amir Rad (researcher).
The researchers have so far found that the FTT-NIRS technology was able to save tissue flaps approximately 85 per cent of the time compared to an average of 48 per cent of the time with a clinical exam alone. In one instance, the FTT-NIRS sensor detected a sustained 15-minute decline in flap blood oxygenation consistent with an obstruction.
“Prompted by the FTT-NIRS warning signal, the clinical team visited the 79-year-old study participant who had inadvertently fallen asleep in a position that compressed the flap blood flow,” shares Shadgan. “Following repositioning and supportive care, blood circulation was restored, saving the flap.”

With these promising results, the research team is pursuing additional research and upgrades to the technology, including a wireless version to better support ease of use in clinical environments.
“Because of its implantability and waterproofing, this type of sensor could have applications in organ transplant monitoring and in other cases involving, for example, the monitoring of tissues damaged from trauma following a car accident,” says Anderson. “We have a few more adjustments to make, but we are getting very close.”
The research team also includes Dr. Oleksandr Butskiy, a head and neck surgeon and clinical assistant professor in the Department of Surgery at UBC, and Amir Rad, a PhD student in the School of Biomedical Engineering at UBC.