
A novel approach to profiling bladder cancers uncovers new biological subtypes of the disease, paving the way for enhanced personalized medicine.
A new study is the first to examine the complete proteome — the full set of proteins — in muscle-invasive bladder cancers (MIBCs) before and after chemotherapy treatment. Published in Nature Communications, Vancouver Coastal Health Research Institute researcher Dr. Peter Black’s study, led by researcher-scientists Drs. Alberto Contreras-Sanz and Gian Negri, uncovered clues to treatment resistance and response.
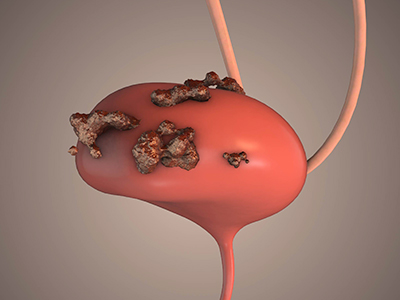
Deadly in approximately half of cases, MIBCs are an important target for precision treatment discovery, states Black.
“We have identified proteins that could help predict which MIBCs resist or respond to treatment, opening a whole new avenue of investigation,” Black shares. “Over the longer term, these findings could help us better understand why some types of MIBC react differently to chemotherapy, potentially leading to new targets for drug development.”
For their research, Black and his team analyzed 143 tissue samples from 107 patients with MIBC prior to them receiving neoadjuvant chemotherapy (NAC) — a first-line treatment to shrink the size of a tumour — and radical cystectomy, which is the surgical removal of the whole bladder. Sixty-nine tissue samples were also collected from the radical cystectomy specimens after patients received NAC.

Among the 107 patients, 75 were either partial-responders or non-responders to NAC.
“We know that around 40 per cent of patients will respond well to NAC, while another 60 per cent of patients will still have MIBC when their bladder is removed,” Black shares. “The question remains whether we can predict which patients will benefit from chemotherapy versus those who will not, and why the therapy is not effective for some individuals.”
The proteome represents a new frontier for research and treatment discovery
The proteome of MIBC tissue samples contains roughly 10,000 proteins responsible for pathological and physiological processes within these tissues, all of which follow genetic instructions taken from DNA within the body’s cells. While prior research has explored the roles of DNA and ribonucleic acid (RNA) in MIBC, the proteome represents a new avenue in MIBC research. Both DNA and RNA perform essential biological functions in regulating or directing processes in cells, including protein production and function.
“Research has defined biological subgroups of patients with MIBC that are associated with distinct clinical outcomes and responses to NAC and/or other treatments,” Black explains. “However, an analysis of the proteome is necessary to guide us to clinically useful proteins that can be targeted by medications.”

After processing the full proteome of MIBC tissue samples, researchers integrated their proteomic data with transcriptomic analyses of RNA expression within tissue samples, zeroing in on pre-treatment protein expression that was associated with subsequent response to NAC. They also analyzed proteins that were depleted or enriched after NAC compared to pre-treatment.
Their results revealed four distinct proteomic clusters pre-NAC and four post-NAC. These could help researchers identify potential prognostic and predictive biomarkers, along with proteins to target with drugs to overcome chemotherapy resistance.
“These findings might give us a hint as to why some MIBC tumours are resistant to treatment.”
Several proteins found to be enriched in a cluster of patients following treatment could be potential targets for new medications and more personalized therapies, states Black. The team also found that patients who had high MIBC cancer cell proteome heterogeneity prior to receiving NAC tended to have poorer outcomes.
“Our next step is to narrow down to a smaller number of defining proteins in each cluster of patients to aid in the classification of these cancers,” says Black. “Advancing precision care also requires the further streamlining of processes to identify patient clusters, as well as the development of novel targeted therapies to treat each cluster.”
“To further validate the predictive capacity of our approach, we are presently expanding our research to, for example, include patients who did not receive chemotherapy.”


